Botulinum toxin is regarded as a 3rd line treatment for patients for overactive bladder (OAB) i.e. after medications and bladder retraining with pelvic floor physiotherapy have been unsuccessful in controlling symptoms.
Patient are regarding as having “refractory” symptoms (i.e. symptoms that are poorly responding to the initial treatments for OAB) when they have not responded to or do not tolerate at least 2 of the newer medications available for OAB symptoms.
What is Botulinum Toxin?
Botulinum toxin (“Botox®” manufactured by the company Allergan®) is a natural, purified protein, which has the ability to relax the muscle into which it is injected. Botulinum toxin type A is produced by a bacteria (known as Clostridium botulinum) similar to the way that penicillin is produced by a mould.
While there are many different types and brands of Botulinum toxin, Botox® is the brand that has been most widely researched for use in the urinary tract.
Botulinum toxin has been widely and safely used for over 20 years in other conditions such as the treatment of squint, muscle spasm, recurrent migraines and more recently by cosmetic surgeons in the treatment of facial wrinkles.
How does Botulinum Toxin work?
Botulinum toxin acts on the nerves that send messages to the bladder muscle telling the bladder muscle to contract. It also acts on the nerves that take the signals of sensation from the bladder to help reduce urgency.
As a result Botulinum toxin helps “relax” the bladder muscle and has been shown to be very effective in reducing symptoms of frequency, urgency and urge urinary incontinence as well as improving quality of life.
The effects of Botulinum toxin eventually wear off after which the muscles return to their normal strength. The duration of action of Botulinum toxin varies from person to person but most studies show that it lasts between 6 to 9 months when used in the bladder.
Who is a candidate for treatment with Botulinum Toxin (Botox®)?
People who have not responded to (or cannot tolerate) medications, bladder retraining and pelvic floor physiotherapy for their overactive bladder (OAB) symptoms are potential candidates for treatment with Botulinum toxin.
People who have neurological problems with their bladder (also called a “neurogenic bladder”) may benefit from treatment with Botulinum toxin.
The use of Botulinum toxin is contra-indicated in people with certain neurological conditions such as Myasthenia Gravis or Motor Neuron Disease, and in pregnancy or when breastfeeding.
Part of the assessment before treatment with Botulinum toxin is a urodynamic study both to help confirm the diagnosis and suitability for this treatment.
Botulinum toxin is NOT effective in treating stress urinary incontinence which is leakage associated with a rise in abdominal pressure e.g. due to cough, sneeze and exercise.
What does treatment with Botulinum Toxin involve?
Treatment with Botulinum toxin involves a day case procedure in hospital or a day procedure unit with the use of either general or local anaesthesia.
The recommended dose of Botulinum toxin (Botox®) for OAB is 100 Units whereas the dose recommended in people with neurological problems (“neurogenic bladder”) is 200 to 300 Units.
A cystoscope (fine telescope connected to a camera) is passed into the bladder through the urine pipe (urethra) and is used to inject the solution of Botulinum toxin. Tiny amounts of diluted Botulinum toxin solution is injected directly into about 20 to 30 locations inside the bladder muscle using a fine needle.

Muscular wall of inside of a bladder due to OAB.
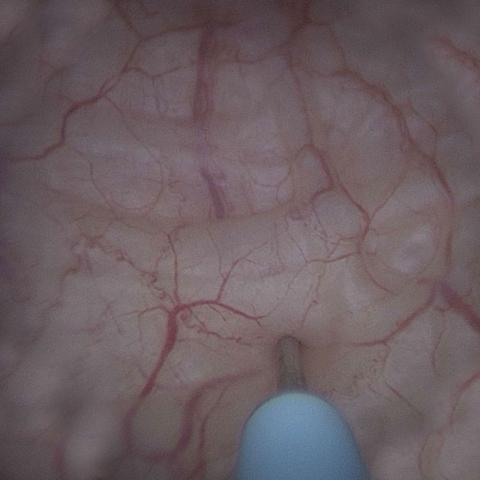
Botulinum toxin solution is injected directly into the bladder muscle using a fine needle under guidance of the cystoscope.

Bladder appearance immediately after injection with Botulinum toxin solution.
The procedure has minimal side effects and patients are discharged home quickly after the procedure.
It is important to realise that the effects of the treatment with Botulinum toxin are NOT immediate and become apparent within 1 to 2 weeks.
A review appointment is made within 1 to 2 weeks after the treatment with Botulinum toxin to check bladder emptying (using an ultrasound in the consulting rooms).
Advantages of treatment with Botulinum Toxin
Botulinum toxin is a minimally invasive treatment for refractory OAB that is extremely well tolerated with a rapid onset of action.
Studies have shown that about 2/3 of patients will benefit from treatment with Botulinum toxin with the benefits lasting usually about 6 to 9 months.
Potential side effects of treatment with Botulinum Toxin
Like all medications Botulinum toxin can have potential side effects.
- Burning and blood in the urine – may be noticed immediately after the procedure but settles very quickly and can be managed with Ural® sachets and paracetamol.
- Urinary tract infection (UTI) can occur after treatment with Botulinum toxin.
- This risk is minimised by giving a dose of antibiotics at the time of the procedure and potentially after the procedure, as well as checking that no bacteria are present in the urine with a MSU (mid stream urine specimen) a few days before the procedure.
- UTI can easily be treated with antibiotics.
- In some people the treatment with Botulinum toxin can work “too well” and potentially result in problems with the bladder not emptying well or inability to pass urine.
- In people with overactive bladder symptoms (OAB) who empty their bladder well before treatment, studies showed that about 6% of patients had difficulty with bladder emptying requiring a treatment known as ISC (intermittent self-catheterisation).
- Intermittent self-catheterisation (ISC) involves passing a tiny tube into the bladder to empty it. This is a simple and safe procedure.
- Although the rate of potentially requiring ISC is very low, people who wish to consider treatment with Botulinum toxin need to be able and willing to learn ISC (taught by a specialist Urology Nurse) or accept a temporary indwelling catheter.
- If needed, ISC is temporary as the effect of the Botulinum toxin wears off and bladder contractions return.
- The vast majority of patients with OAB who receive treatment with Botulinum toxin do not need to perform ISC after the procedure.
- If treatment with Botulinum toxin is successful, retreatment is required as the effect of the Botulinum toxin reduces gradually with time. Every individual is different and it is not possible to predict how long the effect of Botulinum toxin will last in each person. Most commonly the effects of Botulinum toxin last 6 to 9 months.
- To date there does not seem to be a reduction in the effectiveness of Botulinum toxin with retreatment.
- There is not a limit on the number of retreatments that can be performed with Botulinum toxin
- Retreatment can be performed 3 months or more after the last injection of Botulinum toxin if needed.
TGA approval and PBS listing for Botulinum toxin in Australia
Botulinum toxin treatment has been approved by Medicare in Australia for certain selected patients experiencing urinary symptoms, which have not responded adequately to treatment with medication in cases of:
- Neurogenic bladder due to spinal cord injury, Multiple Sclerosis and Spina Bifida as well as
- Idiopathic (i.e. where a cause has not been identified) overactive bladder





